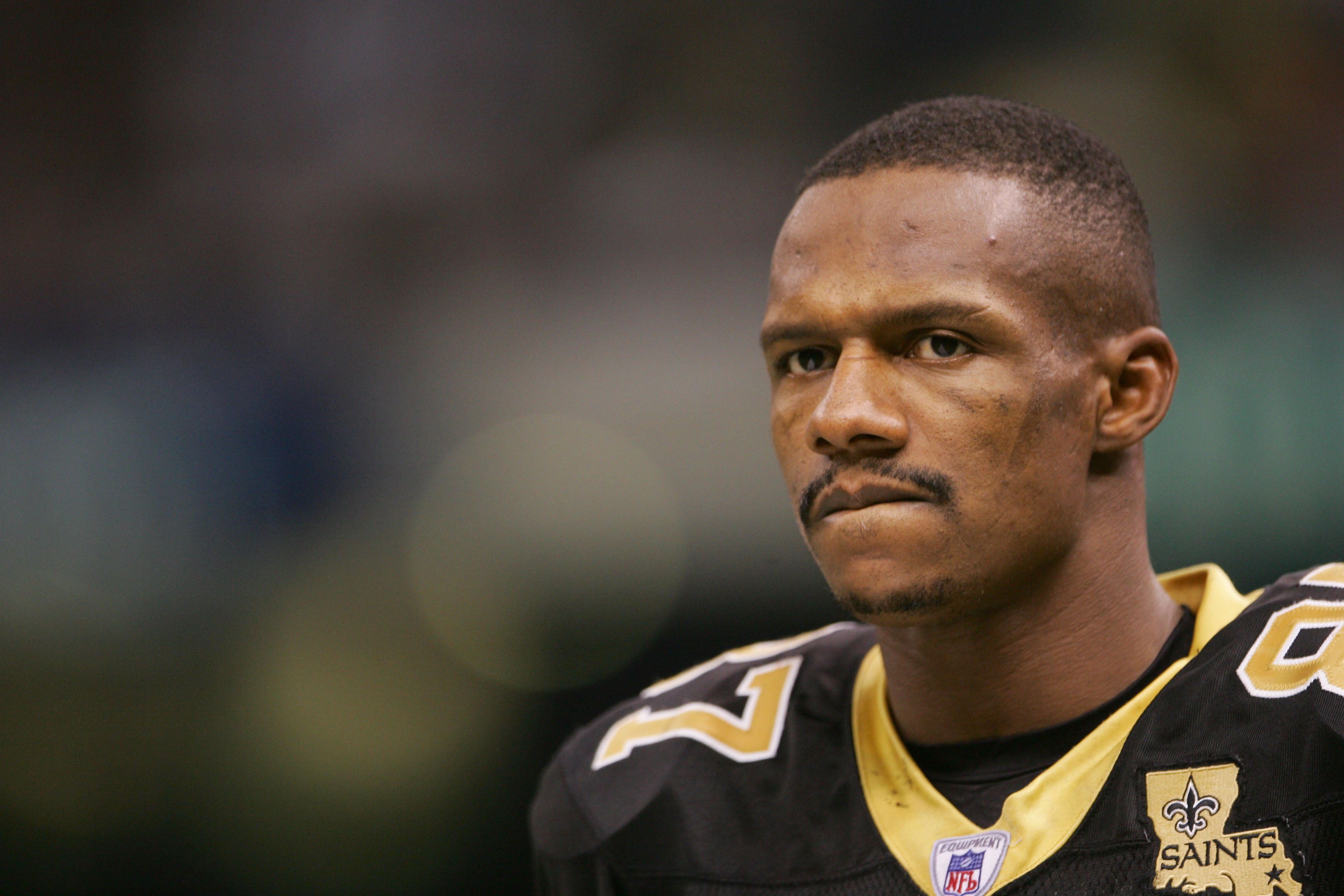
NEW ORLEANS – According to TMZ, Former Saint Joe Horn pleaded guilty to his part in the NFL health benefits scam.
Officials say instead of fighting the case in court, 47-year-old Horn agreed to plead guilty on Thursday to one charge of conspiracy to commit health care fraud.
According to court docs obtained by TMZ Sports, the charge carries a sentence of up to 10 years behind bars, as well as fine of up to $250,000 — plus probation.
But, it seems Horn took the plea deal with the hopes a judge will take it easy on him at his sentencing hearing later next year.
As for the details of the plea agreement — according to the docs, Horn admitted to submitting two false claims that totaled up to $149,775 … and will have to pay that back.
But Joe Horn was not alone in the scam.
In total, 12 retired players are accused of defrauding the league’s retiree health care benefits plan for more than $3 million, according to federal prosecutors.
Ten retired NFL players were charged in two indictments for allegedly submitting phony health care claims seeking to be reimbursed for expensive medical equipment that was never purchased, prosecutors said in a press release. The Department of Justice said it also plans to file charges against two other retired players.
The scheme, which lasted from June 2017 to December 2018, led to over $3.9 million in false and fraudulent claims, of which the plan paid out more than $3.4 million, prosecutors said in a news release.
“Ten former NFL players allegedly committed a brazen, multi-million dollar fraud on a health care plan meant to help their former teammates and other retired players pay legitimate, out-of-pocket medical expenses,” Assistant Attorney General Brian Benczkowski said in a statement.
Four former players were arrested and six agreed to turn themselves in, Benczkowski said.
The defendants include:
- Portis, the former Washington Redskins and Denver Broncos running back;
- Robert McCune, a former linebacker with the Redskins;
- John Eubanks, a former cornerback with the Redskins;
- Tamarick Vanover, a former Kansas City Chiefs wide receiver;
- Ceandris “C.C.” Brown, a former Houston Texans safety;
- James Butler, a former New York Giants and St. Louis Rams safety;
- Fredrick Bennett, a former Houston Texans defensive back;
- Etric Pruitt, a former defensive back for the Atlanta Falcons and Seattle Seahawks;
- Carlos Rogers, a former Redskins and San Francisco 49ers cornerback;
- Correll Buckhalter, a former Philadelphia Eagles running back.
In addition, the government plans to file criminal informations charging Joe Horn, the former New Orleans Saints wide receiver, and Donald “Reche” Caldwell, the former San Diego Chargers and New England Patriots wide receiver, with conspiracy, according to the news release.
McCune is charged with conspiracy, nine counts of wire fraud and nine counts of health care fraud. Eubanks, Vanover and Rogers are charged with conspiracy, two counts each of wire fraud and two counts each of health care fraud. Portis, Brown, Butler and Bennett are charged with conspiracy, wire fraud and health care fraud. And Buckhalter and Pruitt are charged with one count each of conspiracy.
The Gene Upshaw NFL Player Health Reimbursement Account Plan was established as part of the 2006 collective bargaining agreement between the NFL and the NFL Players’ Association. It is intended to provide tax-free reimbursement of out-of-pocket medical expenses not covered by insurance for former NFL players, their wives and their dependents, prosecutors said.
According to the indictments, the former players submitted phony claims for expensive equipment, including hyperbaric oxygen chambers, ultrasound machines designed for a doctor’s office to conduct women’s health exams, and electromagnetic therapy devices for horses.
The claims were for about $40,000 to $50,000 each, prosecutors said. They relied on fabricated invoices, prescriptions and letters of medical necessity, prosecutors said.
In addition, some defendants recruited other retired players to participate in the scheme in exchange for kickbacks and bribes that ranged from a few thousand dollars to $10,000 or more per claim, prosecutors said.
McCune and Buckhalter even called the health benefits plan’s phone line and impersonated other players to check on the status of the claims, the press release states.
Health insurance company Cigna flagged anomalies in the types of claims being filed and referred the fraud to federal investigators, Benczkowski said.
More than 20 FBI field offices across the country participated in the fraud investigation, from Miami to New Jersey to Los Angeles, prosecutors said.


